GENERAL MEDICINE E BLOG
General medicine
Sreeja K
Roll no:168
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient centered online learning portfolio and your valuable inputs on the comment box
Case scenario:
70 years old male daily wage labourer by occupation came to the casuality with
C/O SOB with wheeze since 2 years .
Chief complaints:
PEDAL EDEMA
FACIAL PUFFINESS since 6 months on and off .
Shortness of breath with wheeze since 2 years.
History of present illness:
Patient was apparantly asymptomatic 2 years ago then patient developed on and off sob associated with wheezing associated with dry cough since 2 years , and used to go to local RMP and take medications .
Since last 6 months patient complaints of pedal edema gradually progressive with facial puffiness used some medication and on taking that medications pedal edema got subsided.
Since last 2 months sob aggrevated ( grade 2 to grade 3 ) and associated with orthopnea , PND , episodes of sweating , shivering , giddiness on and off .
No h/o chest pain , palpitaions , fever , decreased urine output .
No loss of appetite .
Non diabetic, non hypertensive
PERSONAL HISTORY:
Marital status - married
Occupation - daily wage labourer
Appetite - Normal
Diet - Mixed
Bowel and bladder movements - regular
Addictions -
Chronic alcoholic since 50 years daily 90 ml.
Chronic smoker since 60 daily 4-5 beedis per day.
No significant family history .
GENERAL EXAMINATION :
Patient is conscious , coherant, cooperative well oriented to time,place,person.
PHYSICAL EXAMINATION:
No pallor , icterus , cyanosis , lymphadenopathy, edema .
VITALS:
BP : 240/120 MM HG
PR : 88/ MIN
RR : 18/ MIN
SPO2: 98% on RA
GRBS : 99 MG %
SYSTEMIC EXAMINATION:
CVS : S1, S2 +
RS : BAE + , NVBS , WHEEZE IN SSA , ISA , INFRA SCAPULAR AREA , SMA , IMA .
P/A : soft , nontender
CNS : NO FND
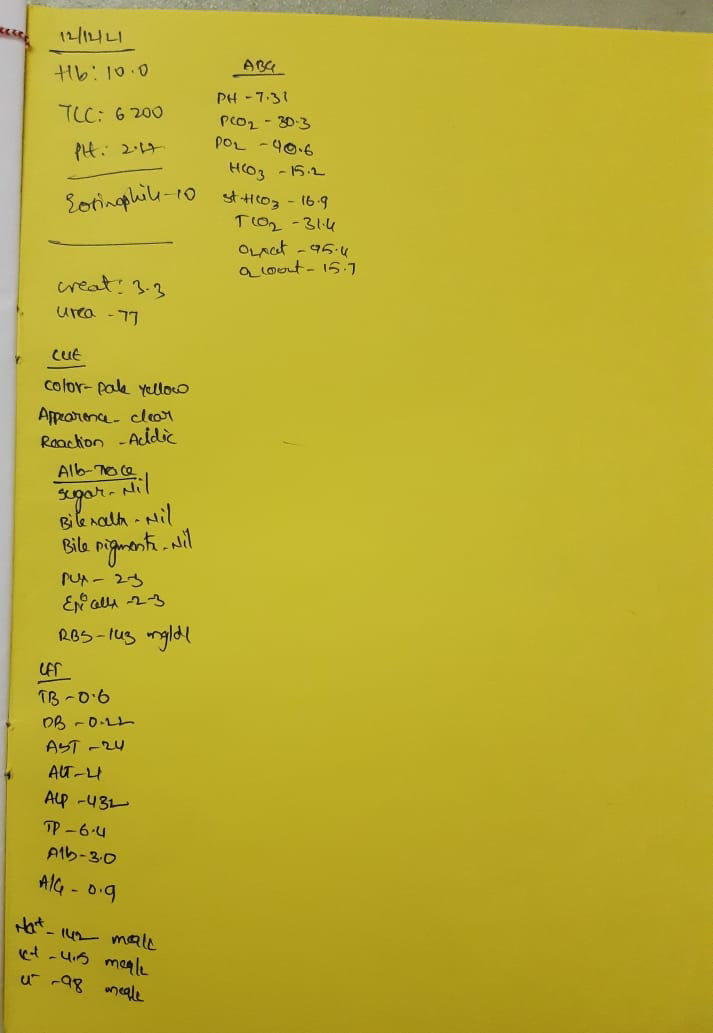
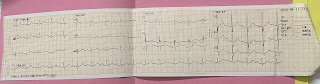
INVESTIGATIONS:
PROVISONAL DIAGNOSIS :
AE COPD WITH? CORPULMONALE
? HEART FAILURE
DENOVO HTN
CKD
Treatment:
1)NEB.DVOLIN
BUDECORT
2)INJ.LASIX 80mg stat given
INJ.LASIX 40mg IV BD
3)TAB.NICARDIA 20mg P.O stat given
4)TAB.CINOD 10 mg P.O BD
5)TAB NODOSIS 500mg PO BD
6)TAB.ECOSPIRIN AV (75/20) PO BD
7)TAB.ACEBROPHYLLINE 100mg PO BD
8)TAB.WYSOLONE 10mg PO BD
9)TAB.PAN 40mg PO BD.






Comments
Post a Comment