A 14 yr old female came with c/o shortness of breath since 2 days
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and prognosis
A 14 year old female resident of Narketpally studying 9 th class came to the OPD with the chief complaints of
CHIEF COMPLAINTS:
Shortness of breath since 2 days
Fever since 1 day.
Abdominal pain since 1 day.
One episode of vomiting 1 day back.
History of present illness : patient was apparently asymptomatic 2 days back then she developed sudden onset of shortness of breath since 2 days gradually progressive grade 4 .Shortness of breath started after patient missed taking insuline dose.
Fever since 1 day high grade associated with chills and rigor relieved on taking medication and no diurinal variation.
Abdominal pain since 1 day in the epigastric region later Progressive to diffuse abdominal pain.
One episode of vomiting non projectile non bilious.
No history of PND,orthopnea,giddiness,loose stools.
History of past illness :
History of 2 previous admissions in the hospital for fever in last 4 years
Known case of diabetes mellitus type 1 since 4 years.N
No H/o HTN TB,asthma,CHD,CVD,eplipsy
No drug allergies.
Family history : History of diabetes mellitus type 1 in the younger sister from 6 years of age.
Personal history :
Sleep : adequate
Diet : mixed
Appetite : normal
Bowel and bladder movements : regular
No history of alcohol consumption, tobacco smoking, tobacco chewing.
General examination :
Patient is conscious, coherent , cooperative well oriented to time, place and person.
Moderately built and nourished.
Pallor : absent
Icterus : absent
Cyanosis : absent
Pedal edema : absent
Lymphadenopathy : absent
Vitals :
BP : 110/70 mm of Hg
Pulse : 120/min
RR :28/min
Temperature : 99 F
Spo2 : 98%
GRBS :126 mg%
System examination :
On abdominal examination:
Inspection:
Shape of abdomen is scaphoid
Flanks are free
Umblicus is in position, inverted
Skin over abdomen normal shiny, no scars, no sinuses, no nodules, no puncture marks.
No visible veins.
No engorged veins.
Movements of abdominal wall are normal, no visible gastric peristalsis.
Palpation:
Liver examination:
On superficial palpation
no tenderness , no raised temperature
On deep palpation
No tenderness in liver
Non pulsatile
Spleen examination:
No tenderness and pain
Percussion :
No fluid thrill
On shifting dullness: tympanic note
Percussion of Liver for Liver Span : 14cm
Auscultation
Normal bowel sounds heard.
2. Bruit - no renal artery bruit heard.
no iliac artery bruit heard.
Respiratory system examination :
Inspection :
Position of trachea central
No dropping of right shoulder
No intercostal indrawing
No supraclavicular hallowness
Shape and symmetry of the chest normal.
No dilated veins.
No visible scars.
accessory muscles of respiration not prominent.
Palpation :
On three finger test : position of the trachea central.
Respiratory movements are normal
On Vocal framitus vibrations are normal.
Ascultation :
Vocal resonence normal
Normal vesicular breath sounds.
Bilateral air entry positive.
No crackles heard.
CVS Examination :
Inspection :
No abnormal palsations
No visible scars.
No chest deformities.
Mediastinum normal
Trachea central in position.
Palpation :
Mediastinal position : apex beat normal
Position of trachea central.
Percussion :
On percussion No cardiomegaly.
Ascultation : S1 and S2 heard. No murmurs heard.
CNS : NAD
INVESTIGATIONS
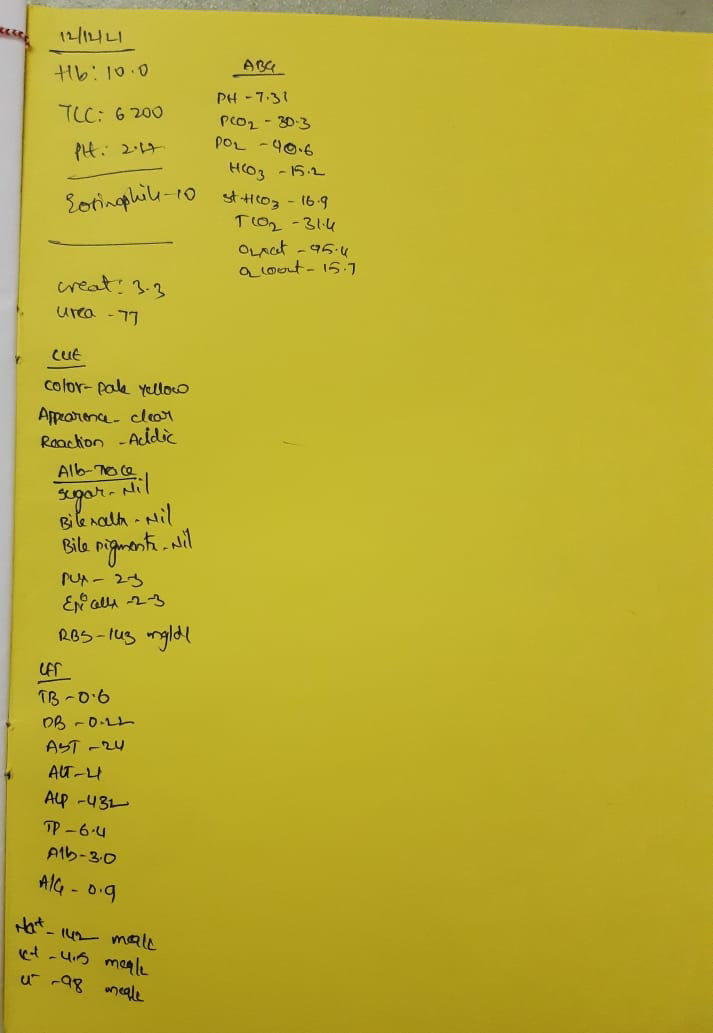
Complete blood picture
Liver function test
Blood grouping
Random blood sugar
Complete urine examination
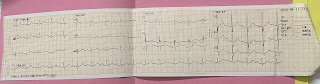
ECG
USG abdomen
Serology
Provisional diagnosis :
Diabetic ketoacidosis with type 1 diabetes mellitus since 4 years.
Treatment :
Injection HAT 5U iv or stat
Iv fluids : 10 NS in first one hour
20 NS 500 ml/h for 3 hours
Maintain GRBS : 150 - 250 mg/ dl
Inform if GRBS greater than or equal to 250 mg/dl and less than or equal to 75 mg /dl
Hourly GRBS monitoring
Monitor vitals hourly and temperature 4 th hourly.
Comments
Post a Comment