A 48yr old male came for dialysis
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
A 48 yr old male with decreased urinary output since 15 days, pedal edema and facial puffiness since 10 days.
HISTORY OF PRESENT ILLNESS-
Patient was apparently asymptomatic 2yrs back then he developed bilateral pedal edema and decreased urinary output. And diagnosed as renal failure.
Shortness of breath G3 insidious in onset and gradually progressive ,pedal edema G2 pitting type
No history of burning micturation
No history of fever
PAST ILLNESS-
History of hypertension
History of diabetes mellitus type 2
No history of asthma, epilepsy, CAD and CVD
PERSONAL HISTORY-
48yr old male married, farmer by occupation has normal appetite, mixed diet, regular bowels, decreased urinary output, no allergies, chronic alcoholic, no history of smoking
GENERAL EXAMINATION-
Patient was drowsy, incoherent and uncooperative
Pallor-
No icterus, cyanosis,clubbing, lymphadenopathy
Vitals-
On presentation-
Temperature-98
BP- 150/90
Pulse rate-95bpm
Respiratory rate-18cpm
GRBS-182mg/dl
SYSTEMIC EXAMINATION-
CVS- S1 and S2 heard, no murmurs heard
Respiratory system- vesicular breath sounds, BAE+
CNS- unconscious speech-normal, no signs of meningitis
Per abdomen- no tenderness, no organomegaly
INVESTIGATIONS-
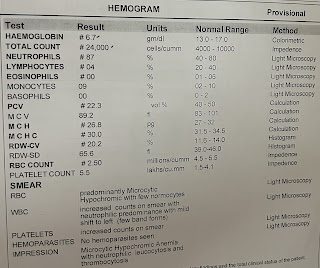
Hemogram
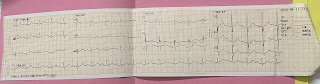
ECG
Ultrasound
Blood grouping and Rh
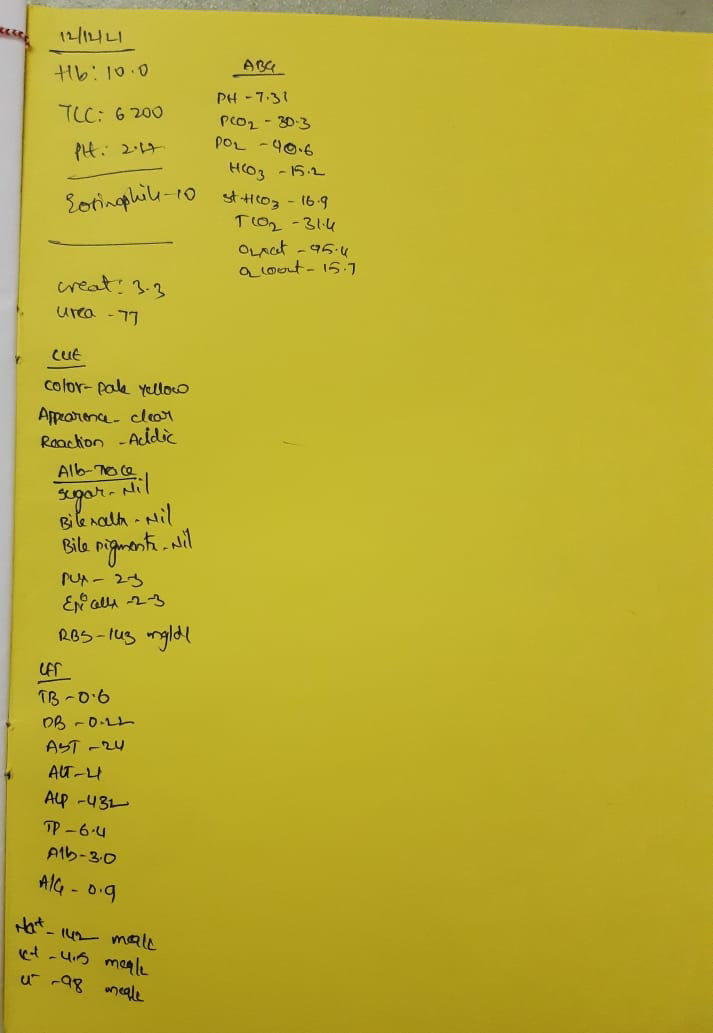
LFT
RFT
SAAG
Serum Iron
PROVISIONAL DIAGNOSIS-







Comments
Post a Comment